In the July issue of JACC Cardiovascular Imaging, our collaborative team from the Piedmont Heart Institute and Georgia Institute of Technology published a paper titled, Quantitative Prediction of Paravalvular Leak in Transcatheter Aortic Valve Replacement Based on Tissue-Mimicking 3D Printing. In this study, we demonstrated the feasibility of using 3D printing technologies to create patient-specific heart valve models that mimic the physiological qualities of the actual valves for pre-surgical planning transcatheter aortic valve replacement (TAVR). Our goal was to improve the success rate of transcatheter aortic valve replacements by selecting the right prosthetic and avoiding a common complication known as paravalvular leakage (PVL).
Tens of thousands of patients each year are diagnosed with heart valve disease. TAVR is often considered for patients who are at high risk for complications with an open-heart surgery to replace the valve. Leakage occurs when the new valve doesn’t achieve a precise fit and blood flows backwards around the prosthetic .
PVL is an extremely important indicator of how well the patient will do short and long term with their new valve. Our research team developed a novel in vitro TAVR pre-procedural planning platform to quantitatively predict the occurrence, severity, and location of post-TAVR PVL.
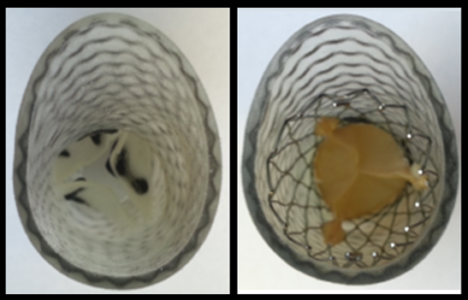
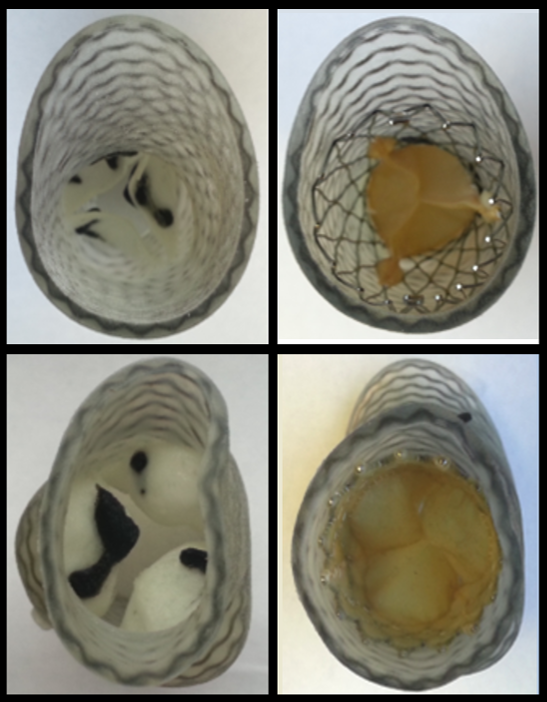
Using PolyJet 3D printing technology (Stratasys, Eden Prairie, MN), we produced 3D patient-specific models incorporating a variety of materials with variant hardness and pliability to replicate visually accurate anatomical models that mimic the tactile feel of aortic tissue. The team made use of the simultaneous multi-material printing ability to embed metamaterial structures during the printing process. Using our proprietary software, we designed directional wavy fibers into the 3D models to mimic the elastic fibers found in the extracellular matrix of human arteries. Creating these models using metamaterial design and multi-material 3D printing takes into account the mechanical behavior of the heart valves, replicating the natural strain-stiffening behavior of soft tissues that comes from the interaction between elastin and collagen, two proteins found in heart valves.
Our next step was to test how the prosthetic valves interact with the 3D printed models to learn whether we could predict leakage. We placed sensors within eighteen models. The sensors enabled us to quantitatively predict the occurrence, severity, and location of any degree of post-TAVR PVL.
The results of this study are quite encouraging. We were able to identify a pre-surgical method that allows us to predict and potentially mitigate the risk of post-TAVR PVL. This will someday allow us to optimize the procedural technique using 3D model surgical simulation and, ultimately, improve patient outcome.
Even though this valve replacement procedure is quite mature, there are still cases where selecting a different size prosthetic or different manufacturer could improve the outcome. 3D printing will be very helpful to determine which one. Among certain high-risk patients, our technique may refine the current approach for the selection of the transcatheter valve type/size, and the selection of the appropriate valve deployment technique, such as the selection of the valve depth and the post-dilatation of the valve, and potentially reduce the rate of post-TAVR PVL.
Eventually, once a patient has a CT scan, we could create a model, try different kinds of valves in the 3D model, and identify which one might work best. We could even predict that a patient would probably have moderate PVL and utilize balloon dilatation to solve it.
The lack of high-fidelity printing materials that mimic the material properties of various soft biological tissues remains a bottleneck for the broader application of medical 3D printing. In addition, the lengthy image segmentation and modeling, the high printing cost, and the lengthy printing and model post-processing all hinder the widespread use of cardiovascular 3D printing. As substantial advancement in the software and hardware of 3D printing is expected in the years to come, these technical obstacles will be eventually cleared and cardiovascular 3D printing will potentially become an essential everyday clinical tool to improve patient care in interventional cardiology.
In the near future, as cardiovascular medicine shifts more towards personalized treatment, I believe 3D printing will play a more important role in patient-specific planning for heart procedures. It will help the physicians better select the right percutaneous device, assess the procedural risk, optimize the deployment technique, and practice for rare and difficult cases in vitro.
SEP 27, 2017 9:51 AM Stratasys